Hearing, balance & the brain
It is not much bigger than a dime. Made up of a meticulous maze of anatomic loops and tubes, hair cells and neurons, and other signaling mechanisms, the ear and vestibular system take in information about the world around us and deliver it to the brain quickly. It is a system that is full of mystery, leaving much for science to explore and explain. However, it is well understood that it does not age gracefully—for adults aged 75 and older, imbalance is the number one cause of doctor visits, and 40 percent experience hearing loss.
Establishing a group to advance science

Researchers at the and Medical Center (URMC) have long been on the quest to understand this system and its parts. Faculty from an array of disciplines, such as Neuroscience, Otolaryngology, , , and , all aim to discover better drug-delivery methods and improve mechanistic and functional understandings of the hearing, balance, and brain connection. The University of Rochester is among the top 20 institutions in the United States in funding for hearing—and balance—related research from the . It is one of the few institutions on that list that does not have a designated center for the group.

“Collaboration has been really key,” said Laurel Carney, PhD, professor of Biomedical Engineering and Neuroscience. “There are no barriers between different groups to get funding that crosses departmental or school boundaries. That is important.”
In 2022, Carney led the group that formally organized nearly 20 faculty members and labs from across the University and Medical Center who study hearing and balance. Known as the Hearing & Balance Research Collective—the group has benefited from its concerted efforts to foster collaboration. It consists of a grant-writing group that has helped faculty secure millions of dollars in funding, a journal club organized by postdoctoral fellows Dana Boebinger, PhD, and Daniel Guest, PhD, that meets weekly to share and discuss new developments and innovations in the field or the research of an upcoming seminar speaker, which is the third component of the Collective.

"Our goals are to teach each other about the various sub-fields within auditory science, and foster community and build relationships,” said Boebinger.
“As a scientist, our journal club has really improved my understanding of a few areas of research that are related to my own but are not in my immediate comfort zone. One good example is physics,” Guest said. “The inner ear is a very complex mechanical system and there is a lot of exciting research, including here at UR and URMC, that is applying new techniques to provide better data on how this system works.”

The Collective’s seminar series has brought several leaders in the field from around the world to Rochester. “The seminar component is key for building our reputation and relationships with some of the leading hearing and balance research,” Kenneth Henry, PhD, associate professor of Otolaryngology and Neuroscience and co-leader of the Collective. “And so far, it has been a great success.”
Meeting unites three labs to ask one question
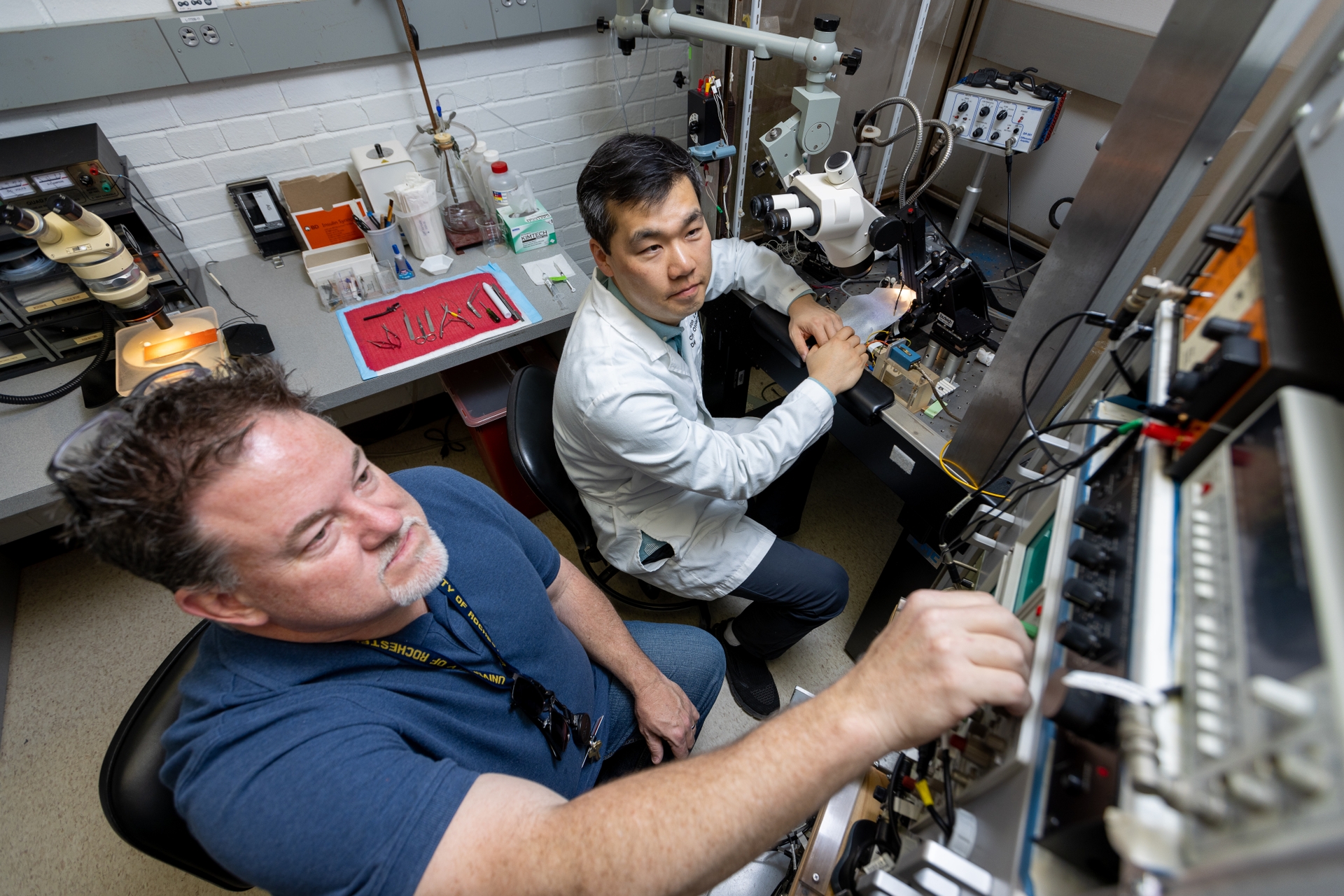
Mechanical Engineering Professor and co-leader of the Collective , had a question but not all the tools he needed. Because of the Collective grant-writing meetings, he knew who may be able to help. Both Carney and Henry immediately responded to the opportunity to collaborate. “Jong-Hoon needed to use some neural measurements to assess the effectiveness of the drug delivery in the inner ear. It is something he could not do in his fluid-dynamics lab,” said Carney. “But we could create the experiments.” Henry and Carney helped develop in-vivo experiments for him to advance his hypothesis. Today, the three are investigators on a project funded by the NIDCD that is looking at whether the inner-ear fluid, which is isolated from all other body fluids, could be a target for drug delivery.

“This project is not trivial,” Nam said, “and it is a great example of the connections built by the Hearing and Balance Research Collective. We need more contact with scientists for this kind of collaboration, and as we mingle, new ideas come. Initially, I did not know if I could begin this experiment, but when I talked to Ken and Laurel, they said this is a feasible experiment and we can start right away. This is a success story.”
Many questions, many labs, one system
The questions being asked by nearly two dozen labs associated with the Collective are sprawling. From the prospect of regenerating hair cells, to treating motion sickness, to how neurons in our brain respond to music.
A discovery in the lab of Neuroscience Associate Professor Patricia White, PhD, also a member of the Collective, is bringing us closer to possibly understanding how and if hair cells can be regenerated. These are the primary cells that detect sound waves and cannot regenerate if damaged or lost in mammals. Her lab found how the activation of the active growth gene, the ERBB2 pathway, happens in mice, which in turn triggers a cascading series of cellular events by which cochlear support cells begin to multiply and activate other neighboring stem cells to become new sensory hair cells. Her lab’s current research is investigating this phenomenon from a mechanistic perspective to determine whether it can improve auditory function after damage in mammals.
J. Christopher Holt, PhD, associate professor of Otolaryngology and Neuroscience, expanded our understanding of how balance stimuli are received by the brain while also offering insights into potential drug targets in the ear, which may be leveraged for treating motion sickness and balance disorders. His study in the efferent vestibular system (EVS) which begins as a small collection of neurons that travel from the brainstem out to the ear where our sense of balance begins, was done in mice. Researchers recorded an increase in the activity of vestibular afferent neurons in mice during stimulation of the EVS system. The excitatory effects of EVS stimulation were diminished by the application of scopolamine, a drug widely used to treat motion sickness in humans, demonstrating for the first time that EVS mechanisms in the ear are also targeted by this drug.
Biomedical Engineering and Neuroscience Associate Professor Edmund Lalor, PhD, uses EEG to understand how the brain allows us to focus on one speaker out of many. His lab discovered the brain is taking an extra step in this processing phenomena. EEG brainwave recordings indicated the sounds coming from the person being listened to were converted into linguistic units known as phonemes, units of sound that can distinguish one word from another, while the other speaker’s sound was not.
Anne Luebke, PhD, associate professor of Neuroscience and Biomedical Engineering at URMC, and Adam Dziorny, MD, PhD, assistant professor of Pediatrics and Biomedical Engineering, considered the role silence may play in hearing preservation. In a 2021 study, they found that a combination of sound and silence may be a key to helping slow the progression of permanent hearing loss. Using intermittent broadband sound, played over an extended period they were able to preserve sensory cells in the ear of mice, while also rewiring some of the central auditory system in the brain, helping preserve the ability to sense the timing of sounds.

The sound of music has a unique relationship to how humans hear. It turns out, there are neurons in the brain that “light up” only to the sound of singing. Samuel Norman-Haignere, PhD, assistant professor of Biostatistics and Neuroscience, was part of this research and helped develop a novel method of measuring the timescale over which different brain regions integrate information. This method is important for understanding the timing and location of how the auditory cortex responds to different sounds. This is integral to learning more about the relationship neurons have to speech and music.

Chair of Otolaryngology Shawn Newlands, MD, PhD, has spent much of his career at the Medical Center. He points to the faculty recruiting under the leadership of Gary Paige, PhD, professor emeritus and former chair of the Neuroscience Department, as the initial push that put Rochester on track to becoming a leader in hearing and balance research. “And we kept building from there,” said Newlands. “We continue to recruit faculty from multiple departments and now with the Collective, we are bringing faculty together regularly in the grant-writing group and engaging with students in a new way through the journal club.”
Recent recruit, Sarah Hayes, AuD, PhD, is an assistant professor of Otolaryngology and co-leader of the Collective, whose research interest aims to understand the adverse effects hearing loss can have on the brain. Specifically, she is investigating the relationship between brain plasticity caused by hearing loss and pathologies such as tinnitus and hyperacusis or the reduced tolerance of sound. “The Medical Center is a very unique setting where I can combine both my passion for helping patients with hearing loss, tinnitus, and hyperacusis, and join a collaborative and vibrant group of hearing and balance researchers,” said Hayes. “As a new faculty member, having the support and guidance from my colleagues in the Hearing and Balance Research Collective has been invaluable as I navigate my career as an early-stage clinician-scientist.”

This article originally appeared in .


